LGBTQ healthcare workers fight to provide gender-affirming care

Nico Olalia had just finished her initial nurse training in the Philippines when she realized her aspirations were growing bigger than her home archipelago.
“There are a lot of trans Filipinos, but they’re always known in the beauty industry, and they’re very seldom found in the professional side,” Olalia said.
So she moved back to the United States, where she was born, for better career prospects. Today, she is a clinical nurse at Cedars-Sinai, one of the largest hospitals in Southern California, where she assists new hires and cares for patients in the neurology division.
Olalia feels like it’s a dream come true; her peers and patients respect her and welcome her contributions. It’s a hope shared by a small but growing number of trans and nonbinary healthcare workers in the U.S.
Yearly surveys of first-year medical students by the Assn. of American Medical Colleges show that the percentage identifying as transgender and gender nonconforming doubled from 0.7% in 2020 to 1.4% in 2023.
These numbers align with the growing LGBTQ+ population in the United States. Today, younger generations are more likely to identify as LGBTQ+ than generations before. A national survey this year found that 28% of Gen Z respondents identified as lesbian, gay, bisexual, transgender or queer.
But that rise in LGBTQ+-identified youths and trans healthcare workers has coincided with escalating restrictions on gender-affirming care.
Between 2022 and 2023, anti-trans legislation proposed across statehouses tripled, with a majority of the bills proposing restrictions on gender-affirming care. According to the Movement Advancement Project, at least half of the states exclude transgender-related healthcare for youths from their Medicaid programs, while only 22 explicitly cover it.
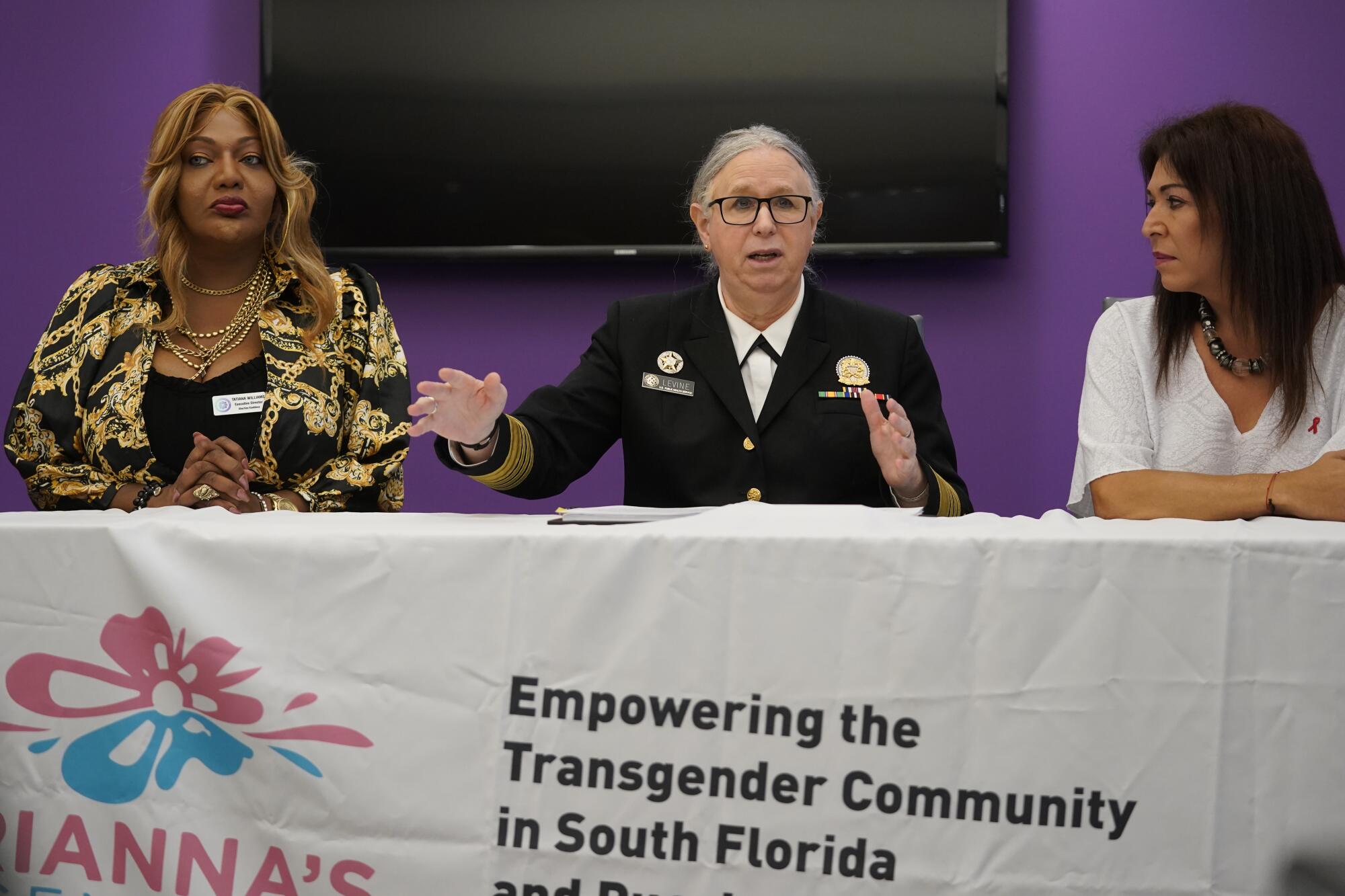
U.S. Assistant Secretary for Health Rachel Levine, center, is shown at a transgender health event in Miami with Tatiana Williams, left, of Transinclusive Group and Arianna Inurritegui-Lint of Arianna’s Center.
(Wilfredo Lee / Associated Press)
“We’ve created medical refugees who have to leave their state to get that care,” said U.S. Assistant Secretary for Health Rachel Levine, the first transgender person confirmed by the Senate to a high government post.
“Transgender medicine can be suicide prevention care. It’s been shown in many studies that it improves the quality of life and can save lives for youth and adults,” said Levine, a pediatrician specializing in adolescent care.
When Levine was doing her medical residency at Mount Sinai Hospital in New York City during the 1980s AIDS crisis, she saw friends and co-workers succumb to the epidemic — an experience that has echoes in the discrimination she sees transgender people facing today, she said.
One study from 2023 showed that 70% of transgender and gender nonconforming patients faced at least one negative interaction with a healthcare provider, ranging from an “unsolicited harmful opinion about gender identity to physical attacks and abuse.” It was only in 2019 that the World Health Organization removed gender dysphoria from its list of mental health illnesses.
Alex Keuroghlian, a clinical psychiatrist at Harvard Medical School, directs training programs through the National LGBTQIA+ Health Education Center that educate healthcare providers across the country on gender-affirming care. They’ve noticed a double standard when it comes to the doubts that people raise against transgender healthcare.
“Given how well resourced anti-trans political groups are, it can really distort the public discourse and make it harder to advance evidence-based, clinically sound practices,” Keuroghlian said of the rampant misinformation they’ve seen online.

Mack Allen, an 18-year-old transgender high school student from Leavenworth, Kan., stands with other young advocates of LGBTQ+ rights after a rally at the state capitol in Topeka, Kan.
(John Hanna / Associated Press)
An uptick in the number of transgender-identifying youths seeking gender-affirming care sparked a theory that “social contagion” was influencing teens to experience “rapid-onset gender dysphoria.” Some practitioners oppose this framing, and research published by the American Academy of Pediatrics has disproved it. Both the American Psychiatric Assn. and the American Pediatric Assn. support gender-affirming care for adolescents.
The news on the legal front hasn’t been all bad for trans healthcare providers; last month, a federal court judge struck down Florida’s law restricting gender-affirming care for minors and adults. However, the practice of categorizing gender in a binary medical system continues.
That’s problematic, said Mauricio Dankers, the intensive care unit director at HCA Florida Aventura Hospital, because the medical erasure of trans people can prevent a proper diagnosis. When doctors have to make split-second decisions in the ICU, he said, failing to recognize a transgender person could prevent them from receiving lifesaving care.
“If I don’t know that a transgender woman may have gone through laryngoplasty to change the tone of her voice, I’m going to go and put the breathing tube [and] I may run into trouble,” Dankers offered as an example. Chest binding used by some transgender people to appear more masculine can also lead to pneumonia if done improperly, he said.

Violet Rin, a transgender woman in Florida, gives herself estrogen injections once a week.
(Francine Orr/Los Angeles Times)
Dankers, a gay immigrant who left Peru for the more tolerant New York City, worries that the politicization of transgender healthcare will put a target on LGBTQ+ healthcare providers.
These restrictions “are going to change how the LGBTQ+ trainee thinks about their career,” Dankers said. He said they might think, “I’m not going to a place where they don’t want me by law.”
After Texas banned gender-affirming care for teens, a pediatric endocrinologist closed her practice and moved out of the state because she feared violence from armed protesters. And this year, a Texas man was sentenced to three months in prison for threatening a Boston physician serving transgender patients.
Fear and violence have had a ripple effect even on states that have enshrined transgender healthcare into law.
Baltimore Safe Haven, a nonprofit that provides transitional housing service focused especially on Black trans women, received an increase of 7,000 calls last year after Gov. Wes Moore signed an executive order protecting gender-affirming medical care in Maryland, according to the Baltimore Sun. Most of the callers lived out of state.

Demonstrators gather on the steps to the state capitol to speak against transgender-related bills being considered in the Texas Legislature.
(Eric Gay / Associated Press)
“I can’t even see my own doctor,” said Jules Gill-Peterson, a transgender woman and associate professor at Johns Hopkins University in Baltimore who studies the history of transgender medicine. Anecdotally, she’s heard of doctors’ caseloads tripling with the slew of requests they receive from new transgender patients.
“It’s only going to put greater pressure on [the] system as people migrate from states where it’s illegal to transition medically to states where it’s not,” Gill-Peterson said.
LGBTQ+ healthcare workers are on the defensive, said Kate Steinle, a queer nurse and chief clinical officer at Folx, a nationwide healthcare provider that serves transgender and queer patients.
“Our general counsel wakes up in the morning and is looking at every single possible legislation that could affect our care,” Steinle said. Folx lobbies the government to ensure that its patients have access to gender-affirming care, but Steinle said fighting anti-trans legislation can sometimes feel like “a game of whack-a-mole” — as one goes down, another takes its place.
Anti-trans legislation is largely symbolic because most of these bills fail, said D Dangaran, a lawyer and director of gender justice at Rights Behind Bars. According to the Trans Legislation Tracker, of the 617 bills introduced, 44 have passed, 348 failed and the rest are pending.
But the fate of transgender healthcare could shift dramatically depending on the outcome of the presidential election in November.
“A Trump presidency will signal to the states another possibility to move forward on all fronts with anti-trans legislation,” Dangaran said. Former President Trump has promised to end gender-affirming care for minors if he wins, and Dangaran anticipates that he would sign “executive orders that are antithetical to protecting trans rights.”

Glenda Starke wears a transgender flag as a counterprotest during a rally in favor of a bill to ban gender-affirming care at the Missouri Capitol in Jefferson City, Mo.
(Charlie Riedel / Associated Press)
Keuroghlian worries that many career government employees in the Department of Health and Human Services could be ousted by political appointees as part of Trump’s ambition to reshape the federal workforce. “There is a lot of important healthcare and research funded by the federal government,” he said.
All of this could reverse the progress that the Biden administration has done to advance gender-affirming care across the country.
“There hasn’t been any president that has more explicitly supported access to gender-affirming care,” said Elana Redfield, the federal policy director at the Williams Institute at UCLA School of Law.
Last week, the Supreme Court agreed to consider the Biden administration’s challenge to Tennessee’s ban on gender-affirming care for teens. The administration argues that the ban violates the 14th amendment’s equal protection clause. A ruling is expected next year that could cement or further erode transgender rights.
Redfield warns that “people who are multiply marginalized are also most affected by these laws,” particularly people of color who live in the Deep South. Beyond the legal restrictions to care, they face problems affording the cost of procedures such as gender-affirming surgery and traveling to where care is available, she said.
Nor can lower-income transgender people afford Folx, a private subscription service that charges $39.99 a month on top of any out-of-pocket costs and copays levied by an insurer.
“Trans people have a lot to tell us about just how bad U.S. healthcare can get,” Gill-Peterson said. “Trans healthcare is not really that different than the rest of healthcare.”

People attend a rally as part of a Transgender Day of Visibility on March 31, 2023, by the U.S. Capitol in Washington.
(Jacquelyn Martin / Associated Press)
Increasing the representation of transgender people in a healthcare system where “profit is placed over people” won’t solve those fundamental inequities, she said. Even if doctors support their transgender patients, Gill-Peterson said, they are still bound by law to follow state regulations and insurers’ dictates.
On the other hand, studies have linked positive health outcomes in LGBTQ+ patients and patients of color to having a healthcare provider who shares their background. That’s one reason University of Michigan medical student Gaines Blasdel, a trans man, wants to become a urologist who can provide gender-affirming surgery to transgender patients such as himself.
Blasdel said gender-affirming care can be an abstract social justice issue to his cisgender classmates, but it isn’t to him. “I’ve been embedded [in medicine] and I’m going to be, no matter how hard it is.”
Jona Tanguay, a physician assistant and medical lead in the medical substance use disorder programs at Whitman-Walker Health in Washington, said it’s important not to discredit the incremental but meaningful progress in the representation and quality of care offered to transgender people.
“Progress isn’t always linear,” they said. Tanguay, who is nonbinary, is also the president of GLMA, formerly known as the Gay and Lesbian Medical Assn. They already see the curriculum expanding and the number of out transgender healthcare providers growing steadily. “Every generation after is going to be more self-aware than they used to be about health disparities.”

Nico Olalia, a transgender woman, moved back to the United States from the Philippines for better career opportunities as a nurse.
(Jireh Deng / Los Angeles Times)
Olalia said her story demonstrates that trans people can practice medicine just as well as their cisgender colleagues. Because she’s also enrolled full time in a nursing doctoral program, her days start at 4:30 a.m., when she wakes up to prepare for her 10- to 12-hour shifts. Her efforts at Cedars-Sinai earned her a prestigious $10,000 no-strings-attached grant from the Simms/Mann Institute & Foundation.
“I do hope that I can have more power to inspire transgender women,” Olalia said. “I want those who are walking behind me to … have that opportunity to go beyond what they’re told to do or what society deems them to be.”
link