Interventions to reduce stress and prevent burnout in healthcare professionals supported by digital applications: a scoping review
1. Introduction
Burnout is a work-related syndrome involving emotional exhaustion, depersonalization, and reduced personal accomplishment (1). In the updated International Classification of Diseases (ICD-11), burnout is listed in the section on problems related to employment or unemployment and is thus now classified as a syndrome. In the workplaces of healthcare professionals, stressors such as a high workload, dealing with suffering patients, and other workplace related conflicts are among the greatest risk factors for developing burnout (2–4). The COVID-19 pandemic has further intensified this psychological burden for healthcare professionals (5, 6). The 2020 Medscape National Physician Burnout and Suicide Report estimated a burnout rate of approximately 43% with women and middle-aged (40–54 years) physicians reporting more commonly symptoms of burnout (7). Estimates of prevalence among medical doctors in Germany vary between 4 and 20%, suggesting much higher values for burnout than in the general population (4.2%) (8). Physician burnout is a global crisis (9). In healthcare professionals burnout not only results in negative health consequences for the individual (10); it also leads to lower patient safety, poorer patient care, lower professionalism, more workplace injuries and higher absenteeism (10–18). The economic impact of burnout among healthcare workers is immense due to increased absenteeism and turnover (19–24), further exacerbating the already acute labor shortage (25, 26).
Current systematic reviews and meta-analyses on interventions for stress reduction and burnout prevention in healthcare professionals have shown that many different interventions are available with varying levels of effectiveness (27–30). Conclusions suggest that individual and organizational solutions are ideally combined to obtain greater improvements in well-being, that interventions should be easily accessible at work, and that digital technologies may be promising support tools in stress prevention (27–30). Comparatively little has been reported regarding detailed intervention characteristics, the digital applications used and how those are integrated into workplace environments. Digital technologies can be a valuable support not only in patient care but also in interventions directed directly to healthcare professionals (31). However, this is needed to further develop the quality of the interventions, especially regarding the integration of digital components.
The goal of this scoping review is to identify current stress reduction and burnout prevention interventions supported by digital components for nurses or medical doctors within workplace health promotion. Of interest were specific programs dedicated to burnout prevention – i.e. in the sense of primary prevention to avoid the development of an illness – as well as programs aimed at reducing stress. Although stress does not per se lead to burnout or other stress consequences, too much stress or not having enough resources to cope can lead to negative consequences (32). These interventions should take place in the context of the general workplace health promotion activities of the respective hospitals. Detailed information on program content, implementation processes, evaluation methods, and relevant endpoints will be provided for further development or optimization of prevention programs in this field. Due to the COVID-19 pandemic situation since early 2020 and the increasing demand for digital applications, the integration of digital applications into interventions is evaluated.
2. Methods
This scoping review adheres to the recommendations from the Preferred Reporting Items for Systematic Review and Meta-Analysis extension for Scoping Reviews (33). A protocol describing rationales and planned methods was submitted to osf.io for registration.
2.1. Eligibility
Inclusion and exclusion criteria were determined based on the research question and discussed in the research team (Table 1). To be included, studies had to evaluate recent workplace health promotion programs using digital components (web-based, digital platforms and apps) for nurses or physicians that were designed to reduce stress or prevent burnout as part of workplace health promotion. Due to the special requirements of these professions, we focused our search on this clientele. Clinical trials from countries in the high-income country context were included assuming that these are provided with similar health care resources. Databases PubMed, Embase, and Psycinfo were searched. Articles published from 2017 onwards have been screened to include only the most recent results. To identify publications that may not have yet been indexed in any of the databases, the search was expanded for Google Scholar limited to the most recent years (≥ 2020).
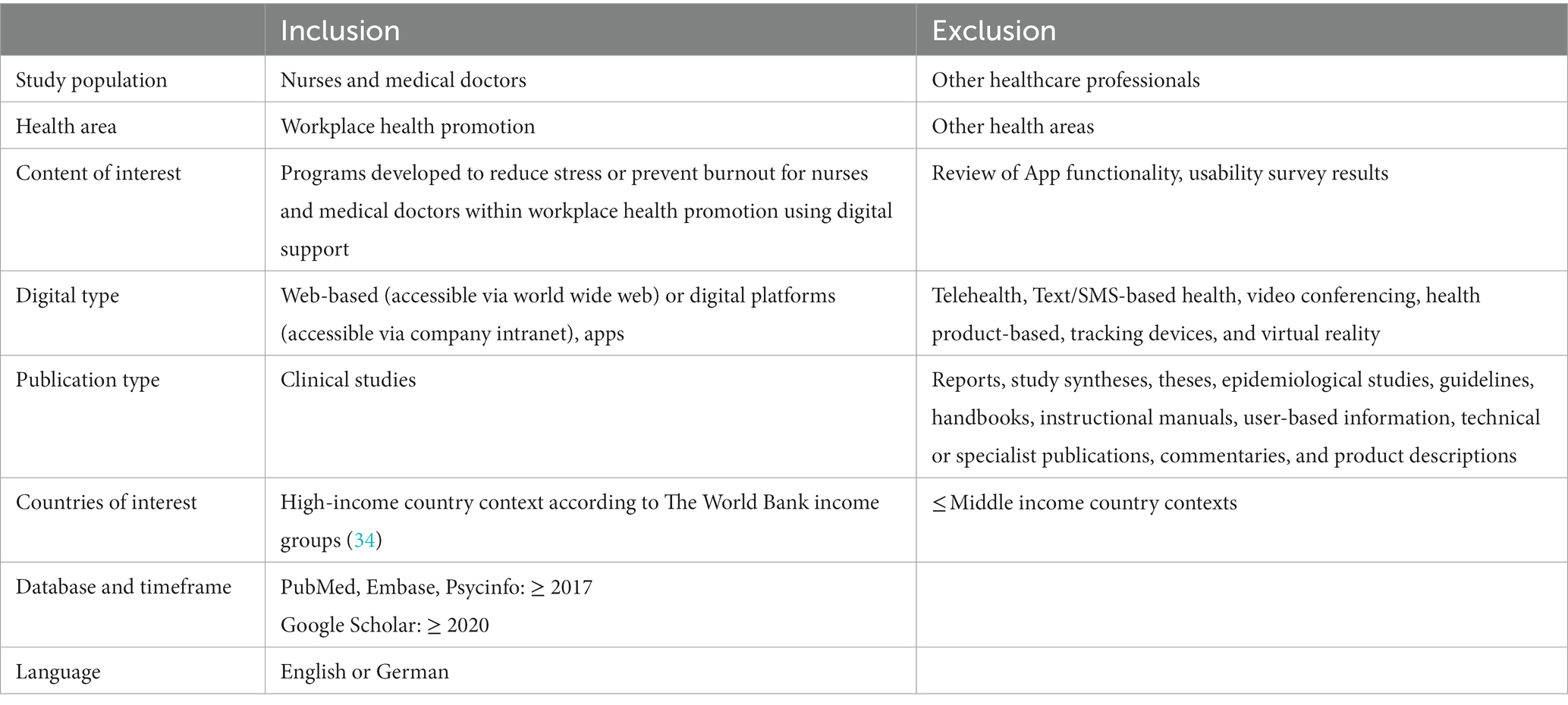
Table 1. Inclusion & exclusion criteria.
2.2. Information sources and search strategy
A search strategy was developed by the research team that consisted of psychologists, physicians and other experienced researchers. The search consisted of associated terms and their keywords, according to the thesaurus of the underlying databases, for “occupational health management,” “stress” or “burnout” (indication), “health care professionals” and “digital component.” A detailed list of German and English search terms and Boolean operators is found in Table 2. PubMed, Embase, PsycInfo, and Google Scholar were searched between 24th and 28th January 2022. A grey literature search on stress prevention projects in hospitals was conducted in parallel but will be published in a separate article due to the limited scope of this review.
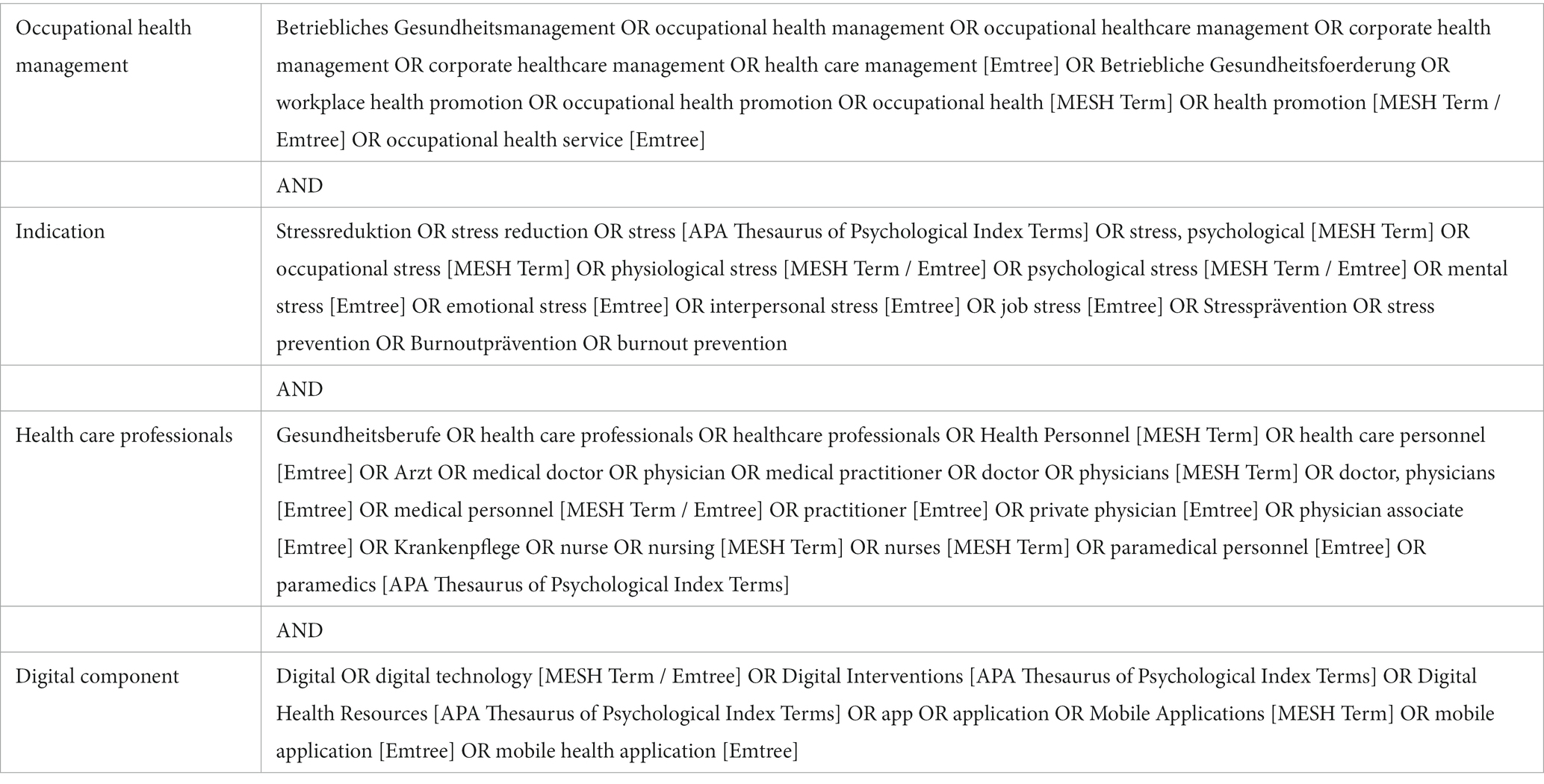
Table 2. Search strategy.
2.3. Data collection and synthesis
Identified publications were imported into EndNote (version 20.2.1), duplicates were removed. Two authors (JB & DA) independently reviewed the abstracts and titles. Then, full-text articles were screened (JB & DA). Two electronic spreadsheets were developed a priori for data extraction. The first form contained data on general study characteristics. The second form contained data on intervention characteristics. JB & DA independently extracted the data into these two spreadsheets. Discrepancies were resolved through discussion between JB, DA, and the rest of the research team. The results of the data extraction, particularly related to the topics of intervention group content/exercise and implications for future interventions, were summarized and discussed by the reviewers (JB & DA) and other members of the research team.
3. Results
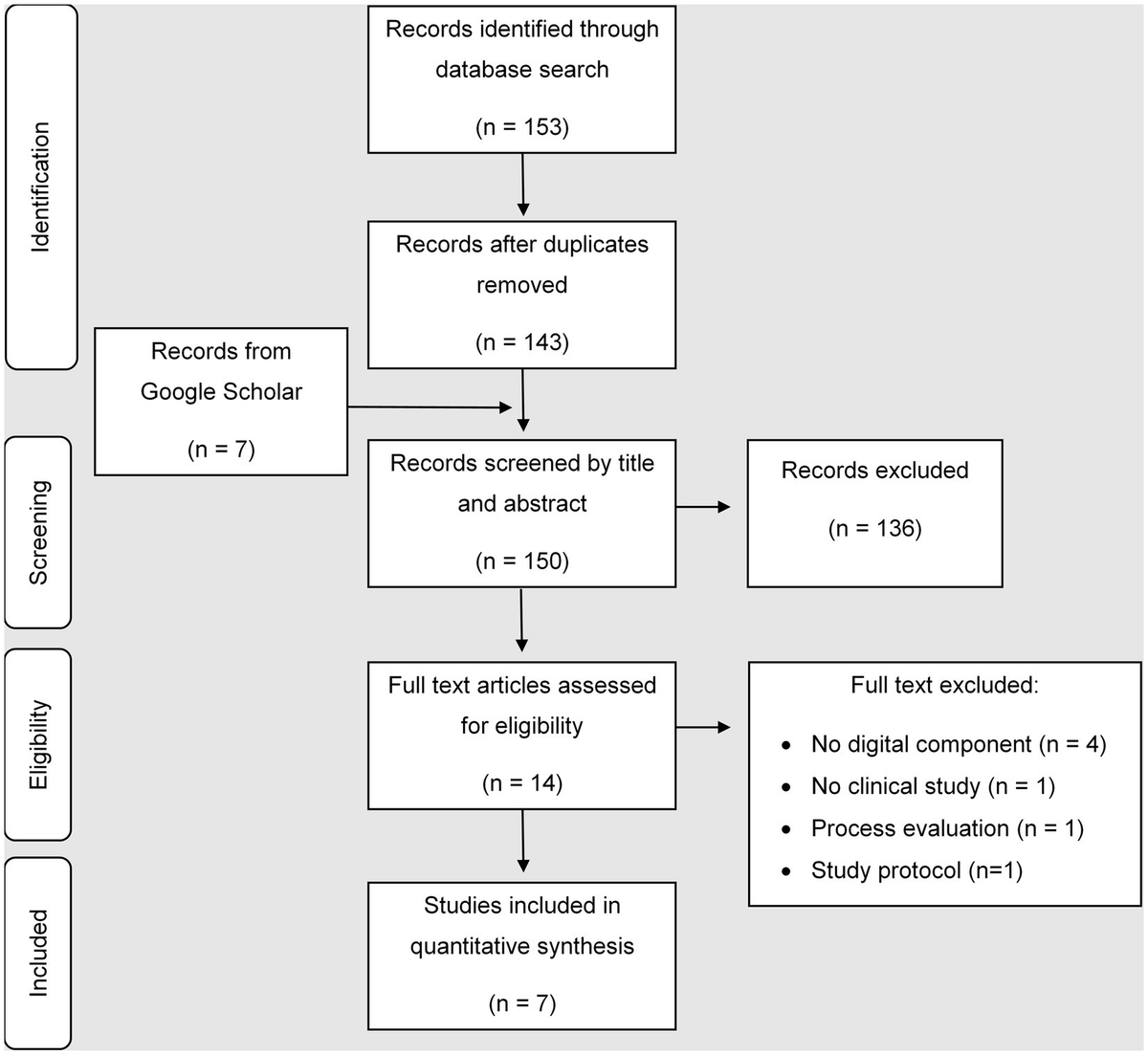
The search strategy identified 153 publications in medical databases. After the removal of duplicates, 143 publications remained. The search in Google Scholar revealed seven additional publications. In total 150 publications were screened by title and abstract. 136 did not meet the inclusion criteria. Fourteen full text articles were screened for inclusion. Seven articles met all inclusion criteria and were used for further data extraction (Figure 1). All publications were original research articles (35–41). Reasons for exclusion of the other seven articles were: no digital component was involved (n = 4) and no primary research article (n = 2) or only a study protocol was published (n = 1). One article described a process evaluation of a study with no results included (42). The primary research article was searched and included into the scoping review (37).
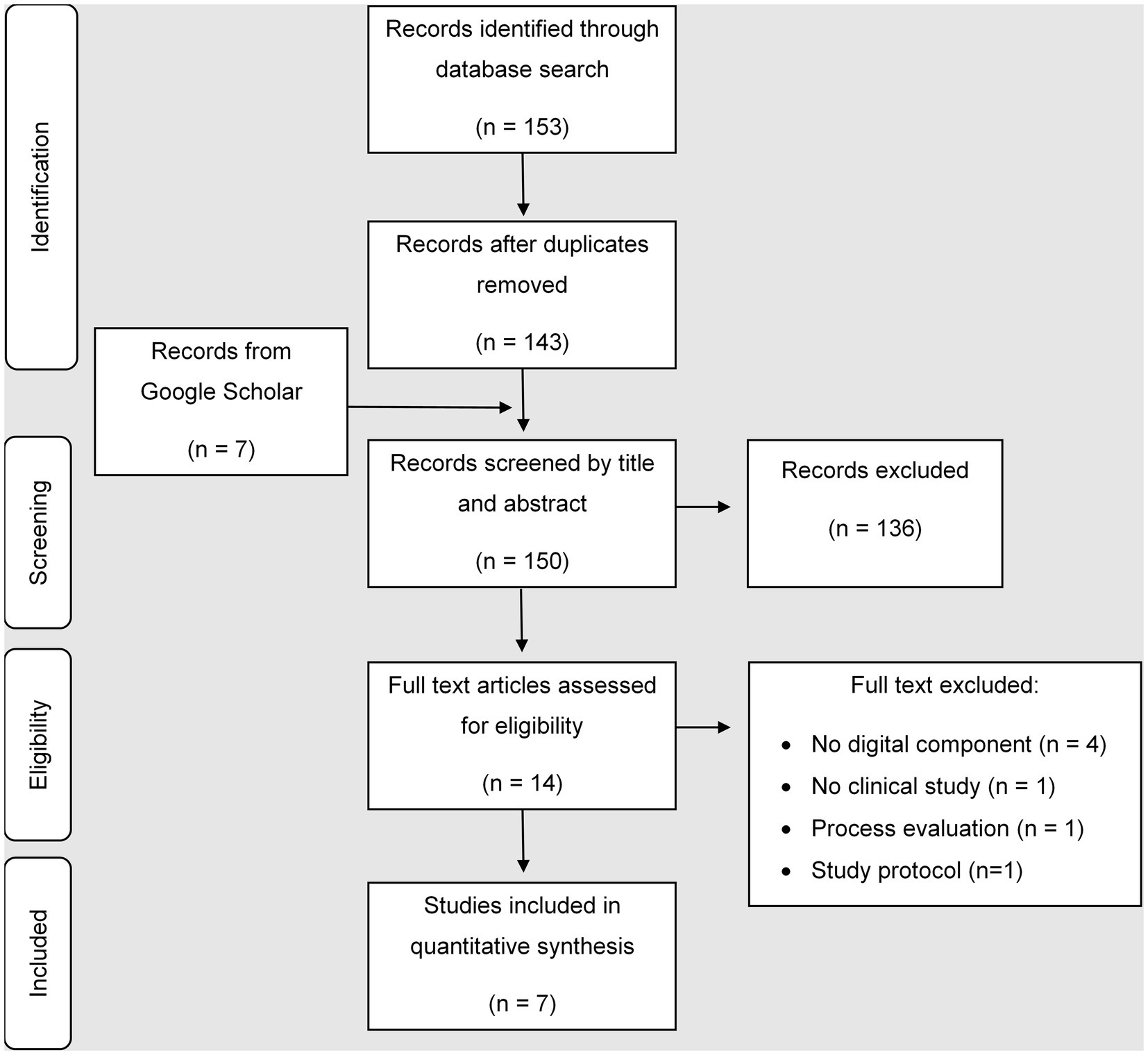
Figure 1. Flowchart.
3.1. Study characteristics
3.1.1. Country
General study details are presented in Table 3. Two out of seven studies were conducted in the USA (35, 39) and two were carried out in Spain (36, 40). The others were conducted in the Netherlands, Poland, and Korea (37, 38).

Table 3. Study characteristics.
3.1.2. Study designs
All studies were published between 2018 and 2021. Four studies used a randomized study design (35, 36, 39, 41). All studies but one had a control group (40). Six out of seven studies included one or more control groups (35–39, 41). Two studies applied a waiting list design (37, 38). Four studies compared the intervention to active control groups (35, 36, 39, 41).
3.1.3. Sample sizes
The sample size in the studies varied between n = 28 and n = 1,200 participants. Three studies had a rather small number of participants per group ≤30 (35, 38, 39). The four remaining studies included between n = 221 and n = 300 participants per group (36, 37, 40, 41).
3.1.4. Outcome measures
A wide range of outcome measures were used. For the primary outcome, three studies used the Depression Anxiety Stress Scale-21 (36, 37, 39), two examined positive and negative emotions with different questionnaires (35, 40) and two focused on stress applying the Perceived Stress Scale (38, 41). For secondary outcomes, two studies used the Maslach Burnout Inventory – Human Services Survey (36, 39) and two made use of the Patient Health Questionnaire (38, 41). Results varied across the different studies and outcome measures.
3.1.5. Results
Results of the Depression Anxiety Stress Scale-21 varied across the studies but were overall positively directed. Fiol-DeRoque et al. (35) found no significant differences between the control and intervention groups but subgroup analyses showed significant improvements among health care workers consuming psychotropic medications and receiving psychotherapy. Havermans et al. (36) analysed a stress subscale of the Depression Anxiety Stress Scale and found that the control group showed higher stress scores than the intervention group over time. Mistretta et al. (39) found significant reductions in stress for the Mindfulness-based resilience training. Further results of the primary and secondary outcomes of the studies are displayed in Table 3.
3.2. Intervention characteristics
Details on the interventions are presented in Table 4.

Table 4. Intervention characteristics.
3.2.1. Intervention content
The interventions were multifaceted and varied across the studies. One study investigated an intervention consisting of expressive writing, adaptive emotion regulation activity, and positive emotion-generation activities (35). Another study investigated a self-managed psychoeducational intervention based on Cognitive Behavioral Therapy (CBT) and mindfulness (36). One study evaluated a multifaceted, integral implementation strategy consisting of a digital platform including information, screening, planning tools and a search engine for interventions to prevent work stress (37). A further study evaluated aspects of mindfulness-based resilience training (MBRT) (39). One study investigated a blended, abbreviated web-based mindfulness-based intervention (40) and another study a self-guided internet intervention containing CBT-framed exercises like (41). One study did not provide details on the intervention used (38).
3.2.2. Duration and intervals of the intervention
Duration and intervals of the intervention exercises varied from 3 min to 4 h and from daily to weekly intervals or intervals chosen by the participants.
3.2.3. Digital components
Four studies worked with digital components for the intervention and/or control group (35, 36, 38, 39). Two studies made use of a web-based platform in different ways: Havermans et al. (37) adopted it to give information on implantation strategies for work stress prevention programs on an organizational level. Smoktunowicz et al. (41) offered a self-guided intervention via the web-based platform. One study applied a blended learning format, which is a combination of face-to-face meetings and online trainings (web-based) (40).
4. Discussion
4.1. Summary of findings
This scoping review shows that the topic of stress reduction and burnout prevention for health professionals is being addressed in recent workplace health management projects that include digital components. It provides information about the individual content, implementation, and evaluation for seven current programs published within the last 5 years with particular attention to the use of digital components, which is of increasing relevance considering the COVID-19 pandemic (31). Content, form of the digital component and the scientific evaluation of the interventions differed fundamentally (35–41). Regarding implementation, it is concluded that brief interventions can be effective, but higher effects might be achieved by higher dose interventions (35, 37, 39) and the behavior of the leader and the characteristics of the team (37) play an important role in project success. Given the scarcity of findings, it is difficult to provide more practical recommendations.
Although interventions for stress reduction and burnout prevention should combine individual and organizational interventions to be as successful as possible (29), this is only partially the case in the studies identified here (37). Individual interventions such as here positive emotion-generation activities (35), self-managed psychoeducational activities (36), MBRT (39) mindfulness (40) or CBT-framed exercises (41) are an important component in the field of stress reduction and burnout prevention, they can hardly bring about sustainable changes on their own. For this, supplementary action at the organizational level is necessary. This is because the main cause of burnout lies in the working conditions of the respective work environment (4). In healthcare professionals, a lack of individual coping mechanisms can promote burnout, but they are rarely the sole cause (4). The fact that stress reduction and burnout prevention still mainly takes place at the individual level, despite better knowledge, raises questions. One reason for this might be that such research and measures are rarely carried out by the most authoritative organizations (43). Research actors usually have no possibility to intervene in existing structures or processes and therefore start where they can: at the individual level. An institutional anchoring of stress reduction and burnout prevention with the backing of management is essential in order to be able to implement organizational measures successfully and sustainably (43).
The results of the evaluated interventions clearly show the challenges faced by program developers: Personnel shortage, turnover, and organizational restructuring hindered the use of the interventions (37) and may be reasons for high drop-out rates (40). Also fear regarding stigma related to mental health issues at work inhibits both treatment and disclosure in physicians (44). The best intervention is of no use if it cannot be implemented in everyday life due to external factors. This must be considered when developing interventions and must not be neglected – an intervention that does not have the support of the executives and management will have a hard time succeeding in the long term. Support from management is not only directly necessary for the success of prevention programs but is also directly related to employee satisfaction. Studies have shown that dissatisfaction with workplace physical health protections was significantly associated with higher levels of emotional exhaustion (45). These problems are also reflected in the high drop-out rates; in one study it was as high as 82.5% (41). Statistical dropout analyses showed that dropouts were related to intervention assignment and occupational and demographic characteristics. Intervention modules that required less time were more likely to be completed. Older workers who had been on the job longer were also more likely to complete the study. These also had higher initial expectancy and higher perceived credibility of the intervention. Interestingly, those who had participated in the intervention had lower baseline scores for work stress, job burnout, depression and work-related post-traumatic stress. This suggests that those who started the intervention already very stressed and with high levels of burnout did not find the time to complete it. Of course, it is those who would benefit the most. Here it is up to the employer, despite acute staff shortages, to create structures that enable participation – at best also in the interventions that take more time. Although high dropouts are not uncommon in non-supervised Internet interventions, this is a particularly high value. The main reasons given for this were initial enthusiasm and curiosity that diminished over time. This is a problem that generally confronts health interventions: How do we ensure that interventions have a lasting effect? Interventions for effective stress reduction and burnout prevention must not be developed detached from the actual context in which they are to be applied later (46). A detailed and comprehensive needs assessment a priori with a targeted view also on the environmental factors of the respective work context is indispensable to be able to develop effective interventions. In the best case, these hindering environmental factors are then immediately integrated into the intervention. These findings complement the calls for a combination of behavioral and situational prevention: for effective stress reduction and burnout prevention, one is not possible without the other (46, 47). The health care system must meet these challenges in a timely manner. The consequences of burnout are severe, not only for healthcare providers but also for patients, as preventable medical errors become increasingly inevitable (10–13, 15, 16). A recent meta-analysis makes this point forcefully using data from 239.246 physicians (11): physician burnout undermines safe health care. Against the background of staff shortages in these important professions, this is once again a matter of urgency. Measures that are effective in practice are necessary and must no longer be regarded as nice-to-have. Without effective stress reduction and burnout prevention firmly anchored in occupational health management, our healthcare system is heading for disaster. The last few years, with the COVID-19 pandemic, have shown how quickly the demands on these professions can intensify again. Effective coping strategies are needed here, including effective stress reduction and burnout prevention programs.
While it is difficult to provide more practical recommendations given the scarcity of findings, the present scoping review illustrates that further research in this area is critically needed; especially regarding micro-interventions, wider samples, longer intervention periods including a passive comparator, interventions on organizational level and blended formats. For comprehensibility of the implementation of programs, they should be described as specific as possible in terms of methodical, didactical and content structure. Also, long-term acceptance (1–2 years perspective) is of importance.
4.2. Limitations
A limitation of the present review is that the quality of the studies included was not assessed; however, this is not required or advised for scoping reviews (33). Also, only seven studies were evaluated in total and thus only five countries reflected. Furthermore, we included only studies from high-income countries in German or English language and only recent publications on clinical studies since the year 2017. However, the overall project included a search for grey literature. It focused on stress prevention projects in hospitals which have not been evaluated in a clinical trial and contains results of semi-structured interviews with project members which gain more insight into this “unpublished” area. The density of information exceeded the scope of this review. Results have been accepted for publication recently (48).
4.3. Conclusion
There is a high demand for comprehensive support of healthcare professionals in terms of long-time mental health (3, 49). This review provides detailed information on the content of current international stress and burnout prevention programs with digital components for health professionals. Both potential barriers and potentially enabling factors related to program content and implementation are identified. The results of this scoping review can be used to inform prevention program development and research in this area. The fact that only seven recent interventions were identified in this scoping review, despite the acute health care burnout crisis, highlights the urgency of developing more programs that are effective, especially in real work settings.
Author contributions
DA, JuS, JB, WS, SR, CK, and GS: conceptualization. DA, JuS, and JB: formal analysis. GS and CK: funding acquisition. DA, JuS, SR, and JB: investigation. DA, WS, and JuS: methodology. DA, AK, MeS, WS, GS, and CK: project administration. DA, AK, GS, and CK: supervision. DA and JuS: writing – original draft. JB, MB, MeS, AK, MaS, JaS, SR, WS, CK, and GS: writing – review and editing. No one was financially compensated for their contribution. All authors contributed to the article and approved the submitted version.
Funding
This review is part of a project funded by a German health insurance company (Techniker Krankenkasse) on burnout prevention among healthcare professionals at Charité – Universitätsmedizin Berlin. The funder has no influence on the contents and results of the present work.
Acknowledgments
We thank Thomas Holm, Nagi Salaz, Lisa Fleischmann, Martina Kringe, Cornelia Schmidt, Jessica Olschewski, Simone Prengel, Alexander Gratopp, Annika Eisermann, Kathrin Altricher, and Bianka Rösner for their valuable feedback. We thank Vanessa Bähr for her support of methodological preparatory work and conceptualization.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Maslach, C, Jackson, SE, and Leiter, MP. Maslach burnout inventory manual. Palo Alto, CA: Consulting Psychologists Press (1996).
Google Scholar
2. Burrows, GD. Stress in health professionals In: R Payne and J Firth-Cozens, editors. Stress medicine, vol. 5. Chichester: Wiley (1989). 130–1.
Google Scholar
4. Maslach, C, and Leiter, MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. (2016) 15:103–11. doi: 10.1002/wps.20311
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Ansari, D. An accumulation of distress: grief, loss, and isolation among healthcare providers during the COVID-19 pandemic. SSM Ment Health. (2022) 2:100146. doi: 10.1016/j.ssmmh.2022.100146
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Ayanian, JZ. Mental health needs of health care workers providing frontline COVID-19 care. JAMA Health Forum. (2020) 1:e200397. doi: 10.1001/jamahealthforum.2020.0397
CrossRef Full Text | Google Scholar
8. Beschoner, P, Limbrecht-Ecklundt, K, and Jerg-Bretzke, L. Psychische Gesundheit von Ärzten. Nervenarzt. (2019) 90:961–74. doi: 10.1007/s00115-019-0739-x
CrossRef Full Text | Google Scholar
9. The Editorial Board. Physician burnout: a global crisis [editorial]. Lancet. (2019) 394:93. doi: 10.1016/S0140-6736(19)31573-9
CrossRef Full Text | Google Scholar
11. Hodkinson, A, Zhou, A, Johnson, J, Geraghty, K, Riley, R, Zhou, A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. (2022) 378:e070442. doi: 10.1136/bmj-2022-070442
CrossRef Full Text | Google Scholar
12. Fahrenkopf, AM, Sectish, TC, Barger, LK, Sharek, PJ, Lewin, D, Chiang, VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. (2008) 336:488–91. doi: 10.1136/bmj.39469.763218.BE
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Shanafelt, TD, Balch, CM, Bechamps, G, Russell, T, Dyrbye, L, Satele, D, et al. Burnout and medical errors among American surgeons. Ann Surg. (2010) 251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3
CrossRef Full Text | Google Scholar
14. West, CP, Tan, AD, Habermann, TM, Sloan, JA, and Shanafelt, TD. Association of resident fatigue and distress with perceived medical errors. JAMA. (2009) 302:1294–300. doi: 10.1001/jama.2009.1389
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Dyrbye, LN, Massie, FS, Eacker, A, Harper, W, Power, D, Durning, SJ, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. (2010) 304:1173–80. doi: 10.1001/jama.2010.1318
PubMed Abstract | CrossRef Full Text | Google Scholar
17. Shanafelt, TD, Mungo, M, Schmitgen, J, Storz, KA, Reeves, D, Hayes, SN, et al. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc. (2016) 91:422–31. doi: 10.1016/j.mayocp.2016.02.001
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Deckard, G, Meterko, M, and Field, D. Physician burnout: an examination of personal, professional, and organizational relationships. Med Care. (1994) 32:745–54. doi: 10.1097/00005650-199407000-00007
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Karasek, RA. An analysis of 19 international case studies of stress prevention through work reorganization using the demand/control model. Bull Sci Technol Soc. (2004) 24:446–56. doi: 10.1177/0270467604269583
CrossRef Full Text | Google Scholar
21. Maslach, C. Burnout: the cost of caring. Palo Alto, CA: Malor Books (2003).
Google Scholar
23. Ramirez, AJ, Graham, J, Richards, MA, Cull, A, and Gregory, WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. (1996) 347:724–8. doi: 10.1016/S0140-6736(96)90077-X
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Jacobson, BH, Aldana, SG, Goetzel, RZ, Vardell, KD, Adams, TB, and Pietras, RJ. The relationship between perceived stress and self-reported illness-related absenteeism. Am J Health Promot. (1996) 11:54–61. doi: 10.4278/0890-1171-11.1.54
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Velana, M, and Rinkenauer, G. Individual-level interventions for decreasing job-related stress and enhancing coping strategies among nurses: a systematic review. Front Psychol. (2021) 12:708696. doi: 10.3389/fpsyg.2021.708696
PubMed Abstract | CrossRef Full Text | Google Scholar
28. West, CP, Dyrbye, LN, Erwin, PJ, and Shanafelt, TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272–81. doi: 10.1016/S0140-6736(16)31279-X
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Zhang, XJ, Song, Y, Jiang, T, Ding, N, and Shi, TY. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine (Baltimore). (2020) 99:e20992. doi: 10.1097/MD.0000000000020992
PubMed Abstract | CrossRef Full Text | Google Scholar
30. Palmer, J, Ku, M, Wang, H, Crosse, K, Bennett, A, Lee, E, et al. Public health emergency and psychological distress among healthcare workers: a scoping review. BMC Public Health. (2022) 22:1396. doi: 10.1186/s12889-022-13761-1
PubMed Abstract | CrossRef Full Text | Google Scholar
31. French National Academy of Medicine. Against the COVID-19, use digital tools on a large scale. Bull Acad Natl Med. (2020) 204:e61–2. doi: 10.1016/j.banm.2020.05.068
CrossRef Full Text | Google Scholar
32. Demerouti, E, Bakker, AB, Nachreiner, F, and Schaufeli, WB. The job demands-resources model of burnout. J Appl Psychol. (2001) 86:499–512. doi: 10.1037/0021-9010.86.3.499
CrossRef Full Text | Google Scholar
33. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
PubMed Abstract | CrossRef Full Text | Google Scholar
35. Coifman, KG, Disabato, DD, Seah, THS, Ostrowski-Delahanty, S, Palmieri, PA, Delahanty, DL, et al. Boosting positive mood in medical and emergency personnel during the COVID-19 pandemic: preliminary evidence of efficacy, feasibility and acceptability of a novel online ambulatory intervention. Occup Environ Med. (2021) 78:555–7. doi: 10.1136/oemed-2021-107427
CrossRef Full Text | Google Scholar
36. Fiol-DeRoque, MA, Serrano-Ripoll, MJ, Jimenez, R, Zamanillo-Campos, R, Yanez-Juan, AM, Bennasar-Veny, M, et al. A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e27039. doi: 10.2196/27039
PubMed Abstract | CrossRef Full Text | Google Scholar
37. Havermans, BM, Boot, CRL, Brouwers, EPM, Houtman, ILD, Heerkens, YF, Zijlstra-Vlasveld, MC, et al. Effectiveness of a digital platform-based implementation strategy to prevent work stress in a healthcare organization: a 12-month follow-up controlled trial. Scand J Work Environ Health. (2018) 44:613–21. doi: 10.5271/sjweh.3758
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Hwang, WJ, and Jo, HH. Evaluation of the effectiveness of mobile app-based stress-management program: a randomized controlled trial. Int J Environ Res Public Health. (2019) 16:4270. doi: 10.3390/ijerph16214270
CrossRef Full Text | Google Scholar
39. Mistretta, EG, Davis, MC, Temkit, M, Lorenz, C, Darby, B, and Stonnington, CM. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J Occup Environ Med. (2018) 60:559–68. doi: 10.1097/JOM.0000000000001285
CrossRef Full Text | Google Scholar
40. Montero-Marin, J, Gaete, J, Araya, R, Demarzo, M, Manzanera, R, Álvarez de Mon, M, et al. Impact of a blended web-based mindfulness programme for general practitioners: a pilot study: Erratum. Mindfulness. (2018) 9:359. doi: 10.1007/s12671-017-0782-2
CrossRef Full Text | Google Scholar
41. Smoktunowicz, E, Lesnierowska, M, Carlbring, P, Andersson, G, and Cieslak, R. Resource-based internet intervention (med-stress) to improve well-being among medical professionals: randomized controlled trial. J Med Internet Res. (2021) 23:e21445. doi: 10.2196/21445
PubMed Abstract | CrossRef Full Text | Google Scholar
42. Havermans, BM, Boot, CRL, Brouwers, EPM, Houtman, ILD, Anema, JR, and van der Beek, AJ. Process evaluation of a digital platform-based implementation strategy aimed at work stress prevention in a health care organization. J Occup Environ Med. (2018) 60:e484–91. doi: 10.1097/JOM.0000000000001402
CrossRef Full Text | Google Scholar
44. Gold, KJ, Andrew, LB, Goldman, EB, and Schwenk, TL. “I would never want to have a mental health diagnosis on my record”: a survey of female physicians on mental health diagnosis, treatment, and reporting. Gen Hosp Psychiatry. (2016) 43:51–7. doi: 10.1016/j.genhosppsych.2016.09.004
CrossRef Full Text | Google Scholar
45. Pereira-Lima, K, Loureiro, SR, Silveira, ILM, Crippa, JA, Hallak, JEC, Zuardi, AW, et al. Workplace protections and burnout among Brazilian frontline health care professionals during the COVID-19 pandemic. Front Psychol. (2022) 13:880049. doi: 10.3389/fpsyg.2022.880049
PubMed Abstract | CrossRef Full Text | Google Scholar
46. Dreison, KC, Luther, L, Bonfils, KA, Sliter, MT, McGrew, JH, and Salyers, MP. Job burnout in mental health providers: a meta-analysis of 35 years of intervention research. J Occup Health Psychol. GKV-Spitzenverband. (2018) 23:18–30. doi: 10.1037/ocp0000047
CrossRef Full Text | Google Scholar
47. National Association of Statutory Health Insurance Fund. Guideline prevention. Fields of action and criteria according to § 20 Para. 2 SGB V [Leitfaden Prävention. Handlungsfelder und Kriterien nach § 20 Abs. 2 SGB V]. Berlin: Arbeitsmedizin Sozialmedizin Umweltmedizin (2021).
Google Scholar
48. Schiele, JK, Koch, AK, Adam, D, Berschick, J, Schröter, M, and Reschke, R, et al. (in press). From burnout to breakthrough – mental health resilience programs for German hospital professionals: a grey literature review with semi-structured interviews.
Google Scholar
49. Jenkins, R, and Elliott, P. Stressors, burnout and social support: nurses in acute mental health settings. J Adv Nurs. (2004) 48:622–31. doi: 10.1111/j.1365-2648.2004.03240.x
CrossRef Full Text | Google Scholar
link