Patients must be savvy health-care consumers, retired nurse writes

Patricia Baker’s Stone Journey advises keeping meticulous notes with concise, accurate lists of symptoms, dates and times – that’s what she did

Article content
There are times when having an MD or RN after a name can mean more than merely having added advantage in landing solid employment.
Advertisement 2
Article content
Simply put, medical professionals know how the sausage is made when it comes to both the intricacies of the health-care system and, perhaps most importantly, how the human body functions. Or doesn’t.
Article content
Recommended Videos
Article content
But the sad reality for most folks is the fact they don’t have a clue which end is up when it comes to the nuts and bolts of health care, which can be mighty intimidating.
In fact, obtaining care for patients and their families with no medical background can be a nightmare, argues a new book penned by a veteran Sault Ste. Marie nurse.
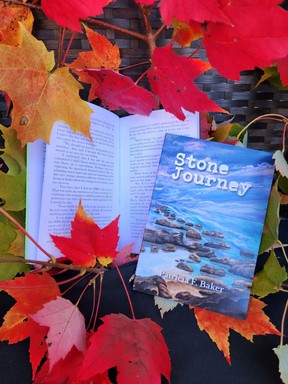
Patricia Baker’s Stone Journey contends medicine is its own language, one that can be Greek – and mighty frustrating – for so many.
“We have the training behind us to listen,” says Baker, a retired Sault Area Hospital nurse, who served the profession for more than five decades. “When we do seek health (care), we have an advantage that, unfortunately, the general public does not have.
Advertisement 3
Article content
“We speak the language. Medicine has its own language. And it’s not English and it’s not French.”
That doesn’t mean the general public has to sit on the sidelines. In fact, Stone Journey, published by Lost Telegram Press and released last summer, argues that proper preparation is key.
Baker says that simply means keeping close track when things seem to be not working well. Recording a concise, accurate list of symptoms, with dates and times, is paramount.
“Pain, no pain … whatever,” Baker said. “Where it is.”
An up-to-date list of medications is also important.
“Don’t just put a whole bunch of pills in a bag and take them and let them figure it out,” said Baker, also suggesting questions to caregives be written in a “concise way.”
Advertisement 4
Article content
Baker, who pens a regular Sault Star column, is not just speaking and writing as a health-care professional. She knows well what it’s like on the receiving end of the system. She kept meticulous journal notes during her cancer journey more than a decade ago, so when she decided to write Stone Journey in 2024, the factual data were there.
A firm grasp of the facts is essential for all concerned.
“That opens up the door to make your conversation concise, accurate, based on facts, and you’re not sitting there being intimidated searching for the right words to talk about,” she added.
“The caregiver is going to have their hand on the doorknob because they have 10 minutes to do all this work and they have 20 people waiting. You can’t fault the health-care providers.”
Advertisement 5
Article content
However pressed the primary caregiver may appear, patients must never think they are a nuisance. Indeed, it’s incumbent they learn how to be their own best advocates.
“If you don’t do it, nobody is going to do it for you,” Baker said.
This former nurse and medical educator knows a thing or two about advocacy, having had her own medical crosses to bear. Not to mention those of her husband, Harry, who died last July following a long period of failing health.
Baker was diagnosed with rectal cancer in January 2013 after a short period of rectal bleeding. For many years she had internal hemorrhoids and didn’t think much of the bleeding at first because she felt healthy.
“The nurse in me kept chattering to get it checked out,” Baker said. “I did.”
Advertisement 6
Article content
A colonoscopy in February 2013 found a malignant rectal tumour 15 centimetres above the anus. Pathology showed stage 1 or 2 cancer.
Baker was admitted to the Algoma District Cancer Program, where diagnostic tests were ordered as well as consultations with medical and radiology oncologists and a surgeon.
Included in this care was an oncologist from Health Sciences North in Sudbury. He strongly recommended surgery to remove a section of her bowel. Baker then had six weeks of radiation, and continuous intravenous chemotherapy. She took a month vacation from treatment and had surgery that April.
A local surgeon performed what is called an anterior resection while removing some local lymph nodes.
Four months after rectal surgery, Baker discovered a lump in her right breast. Ultrasound and biopsy were done, and she was diagnosed with Stage 2 breast cancer in August 2013.
Advertisement 7
Article content
Baker had surgery in early September, then radiation and a return to chemo for rectal cancer.
Treatment was able to put Baker in remission from Stage 3 rectal cancer and Stage 2 breast cancer for 12 years. In fact, she was back to work in early 2014.
Baker’s recent esophageal cancer diagnosis – Stone Journey documents her 2013 cancer journey – was caught early, and Baker, 76, says she now has an “excellent” prognosis.
“They can do wonders in updated treatments today,” she said.
Needless to say, being a patient can bring out less-than-ideal personal traits. A profound lack of patience is common. And understandable.
“When they have to wait 10 hours in an emergency department, they don’t feel important at all. They don’t even feel visible,” Baker said.
Advertisement 8
Article content
“Because when they’re sick and they’re scared, then there is no one else in the waiting room except them. You become focused on you because you may have waited two weeks to get an appointment. You’ve been stewing about it. You think you’re dying.
“It’s almost impossible to rationalize those feelings because we become self-centred. And that’s human instinct because we’re protecting ourselves.”
One way to foster peace between patient and primary caregiver is to maintain mutual respect.
“If you go in there demanding, it’s not going to come over very well,” Baker said. “There are ways of doing things. There are ways of being respectful. If you do become frustrated, there’s ways of being frustrated as well.”
And, if possible, avoid Dr. Google. But if symptoms have been researched online, don’t try to contradict caregiver counsel with web-based chatter, perhaps collected from less-then-trustful sources, Baker suggests.
“Information surrounds us,” she said. “There is too much information. It bombards us. It could be AI. It could be all sorts of misinformation.
“I think it’s a better idea to just write down what you’re feeling.”
Stone Journey is available via Baker’s website www.rainmakerscreativeworks.ca
On X: @JeffreyOugler
Article content
link






