UM Today | Rady Faculty of Health Sciences

November 24, 2025 —
In the 1990s, Dr. Charles Bernstein, distinguished professor of internal medicine at the Rady Faculty of Health Sciences’ Max Rady College of Medicine, found that Canada had the highest rates of inflammatory bowel disease (IBD) in the world. At the time, the disease was predominantly diagnosed in Western countries.
Today, IBD affects populations around the globe, including in developing countries. It affects more than 300,000 people in Canada.
IBD is a chronic digestive condition with no known cure. Crohn’s disease and ulcerative colitis — the two main types of IBD — cause significant discomfort for patients, including abdominal pain, diarrhea, blood in bowel movements and fatigue. In some cases, patients require surgery.
“We don’t know what causes these diseases,” Bernstein said. “We think it’s something in the environment — maybe something we eat or inhale. It could also be linked to things like antibiotic use, which changes the bacteria in our gut and affects how our immune system responds.”
Bernstein led the first global study on health-care spending for IBD, aiming to identify key areas in disease management and highlight gaps in diagnosis, treatment and access to care. The research was recently published in Gastroenterology.
Global IBD trends and treatment disparities
As IBD has become a global issue, the researchers found that symptoms and disease progression are similar across countries.
“Whether you’re in Paris, Delhi, Shanghai or Winnipeg, the experience of living with IBD is surprisingly consistent,” he said.
To better understand global health-care gaps, the team created a survey and sent it to IBD specialists in 85 countries.
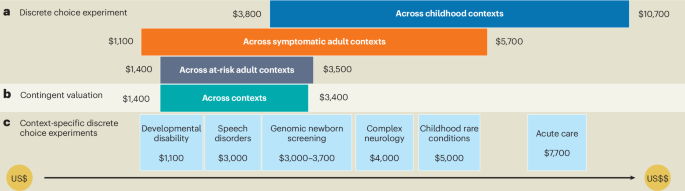
With the help of Julia Witt, an economist at the University of Manitoba, the countries were divided into three tiers based on IBD health-care spending per capita: top spending (Tier 1), middle spending (Tier 2) and lowest spending (Tier 3).
Bernstein in his laboratory at the University of Manitoba’s Bannatyne campus.
“There’s a significant gap in resources. Third-tier countries lack access to state-of-the-art equipment and the kind of diagnostics I use here in Winnipeg,” Bernstein said.
The research team found that limited access to specialty clinics, advanced imaging, expert histopathology and medications remains a challenge in many countries. The medications patients may need to take for 20 years or more cost $20,000 to $40,000 annually in Canada.
While Canada is part of Tier 1, Bernstein said there are still lessons to be learned from countries in other tiers. The study found that doctors in Tier 3 countries are more likely to provide mental health care to their patients, including psychological therapies or medications.
“Manitobans may receive some of the best care in the world, but there are still limitations compared to privately insured patients in the United States,” Bernstein said. “Here, patients may wait a long time for an MRI or face challenges accessing mental health support.”
A call for change
Bernstein said more needs to be done to improve care for people living with IBD. He offered a call to action:
- For policymakers and industry leaders: Understand that IBD is a growing concern. Governments and industry can help by increasing resources and developing more holistic models of care. These models should include not just physicians, but also nurse practitioners, nurses, psychologists and dietitians. Pharmaceutical companies could also explore ways to offer IBD treatments at lower costs in developing countries to improve accessibility.
- For health-care providers: Advocate for patients and lobby health-care systems and governments to improve support. Encourage the development of patient-led support networks and educational resources.
While there is still no cure for IBD, Bernstein said there is hope. He continues to collaborate internationally to improve care for people living with the disease.
“We’re not close to a cure because we don’t know the cause,” Bernstein said. “But we’ve made a lot of progress over the years. It’s satisfying to see how we’re managing patients better and sending fewer to surgery.”
***
Read the full study on Gastroenterology: Global discrepancies in inflammatory bowel disease care reflect healthcare expenditure per capita
link