Early detection of breast cancer: What you need to know

Breast cancer is the most common cancer among women globally and the second most common in the United States. In the U.S., the average risk of a woman developing breast cancer sometime in her life is roughly 13%, or a 1 in 8 chance. However, the five-year survival rate for localized breast cancer – cancer that is contained to the breast – is more than 99%.
Early detection of breast cancer, through regular mammograms or other screening methods, can give people the best chance at effective treatment and can be lifesaving. Knowing what to look for and when to get screened can help catch breast cancer early, when it’s most treatable.
Did you know? Across the HCA Healthcare network, our caregivers perform approximately 1.5 million mammograms each year – an essential tool in the early detection of breast cancer.
Breast cancer screening guidelines
The U.S. Preventive Services Task Force and the American College of Radiology both recommend beginning routine mammograms at age 40. After 55, the American Cancer Society advises screening every other year, though yearly screenings remain a good choice. In general, it’s best to continue mammograms as long as you’re in good health and expect to live at least 10 more years.
The bottom line: always talk with your doctor about the schedule that’s right for you.


“I think a lot of people believe that breast cancer is a disease of older women – and largely it has been in the United States – but we are seeing a rise in breast cancer diagnoses among women under 50, and even under 40,” shared Dr. Kayla Griffith, a breast cancer surgeon at affiliate HCA HealthONE Rose in Denver.
If you’re considered high risk for breast cancer, you should begin annual screenings with both breast MRIs and mammograms around age 30. If you’re unsure about your risk level, talk to your doctor. They can help you complete a risk assessment and decide whether earlier or more intensive screening is right for you.
“Pay attention to your health and don’t hesitate to advocate for yourself,” shared Dr. Griffith. “Too often, women prioritize caring for others and put their own well-being last. But the truth is, taking care of yourself isn’t selfish – it’s essential. You can’t fully care of others if you’re not taking care of yourself first. That includes making time for important screenings like mammograms.”
Personal risk factors for breast cancer
The main risk factors for breast cancer are being a woman and getting older. Most breast cancers are found in women age 50 and older. Other risk factors include:
- Genetic mutations (such as BRCA1 or BRCA2)
- Early menstruation or late menopause
- Dense breast tissue
- Prior breast cancer or certain benign breast diseases
- Physical inactivity
- Long-term hormone therapy
- Heavy alcohol use
- Strong family history of breast cancer
- Chest radiation before age 30
Having a risk factor does not mean you will get breast cancer. But knowing you have a risk factor can help you be prepared and know what to look for. If you are concerned, talk to your doctor about ways to lower your risk.
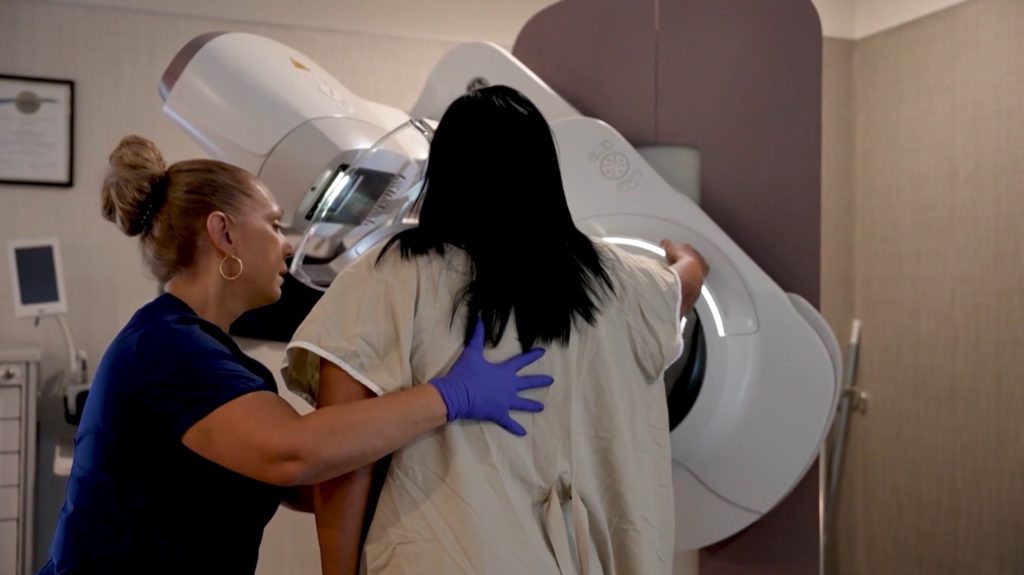
What to expect during a mammogram
There are two types of mammograms:
- A screening mammogram is an X-ray that looks for unsuspected breast cancer in women who do not have symptoms.
- A diagnostic mammogram examines abnormalities, usually after they are spotted on a screening mammogram.
When you show up for your mammogram, you will need to undress just to your waist for your exam, so consider wearing a two-piece outfit. During the screening, each breast is compressed between two plates of a mammography machine. X-rays are taken of each breast from the front and the side.
The pressure and positioning required with mammograms can be uncomfortable. It may help to know that the screening portion of the appointment only takes about 10 to 15 minutes. Diagnostic mammograms can take longer than screening mammograms because more images are needed.
What to check between mammograms
Medical organizations have shifted from formal monthly breast self-exams to encouraging women to simply become familiar with their breasts and how they normally look and feel. This can make it easier to recognize any changes.
To familiarize yourself with your breasts:
- Do a visual inspection in front of a mirror with your hands on your hips and a second with your arms raised above your head. Look for visual changes such as redness, swelling or puckering. Also look for nipple inversion (a nipple that is pushed inward rather than sticking out) or dimpling.
- Manually inspect your breasts for lumps, knots or thickened areas. Gradually increase pressure as you go around the breast and squeeze the nipple to check for discharge. You’ll want to do this twice — while standing up and while lying down. Be sure to cover the entire breast and armpit area.
It can help to explore what your breasts normally feel and look like a few days after your period ends. Hormone levels fluctuate throughout the month, causing changes in breast tissue such as swelling and tenderness.
Know your risk
Talking with your doctor about your personal risk factors, keeping up with recommended screenings and paying attention to changes in your body can lead to early detection of breast cancer and better outcomes.
“You didn’t ask for this. You know, that’s the biggest take home,” Dr. Griffith told Denver7, reflecting on the message she shares with her patients. “We are where we are. You didn’t do anything to cause it. We’re going to get you through it.”
Stories of strength: Kansas nurse faces breast cancer head-on


The story of HCA Healthcare nurse Amy Graf is a powerful reminder that early detection saves lives. When Amy went in for her annual mammogram on Oct. 5, 2023, she didn’t expect life-altering news. Just a year earlier, her results were normal. But this time, the screening and follow-up diagnostics revealed triple-negative breast cancer – a rare and aggressive form of the disease. Amy had no symptoms, no family history and no warning signs.
From the moment of her diagnosis, Amy was surrounded by a compassionate care team at Overland Park Regional Medical Center in Overland Park, Kansas, part of the HCA Healthcare Sarah Cannon Cancer Network. Amy began treatment – undergoing eight rounds of chemotherapy and a double mastectomy with reconstruction. Her body responded fully to treatment, and today, she’s cancer-free. “If anything comes from all of this, I want to advocate for every woman to take advantage of this life-saving screening,” Amy said.
Thanks to that one routine mammogram, Amy is embracing life’s everyday moments – visiting her two college-aged kids at her alma-mater and cheering on her 16-year-old daughter at her soccer games – all with the support of both her family and “work family.”
Related article: Read Amy’s own words as she reflects on her cancer diagnosis, treatment and the meaningful relationship she built with her nurse navigator on HCA Midwest Health’s website.
Stories of strength: How a care team became a patient’s lifeline


When Heather Masters discovered a lump in her breast, she hoped it would disappear. But after weeks of waiting and a series of tests, she was diagnosed with invasive ductal carcinoma – the most common type of breast cancer. That moment in August 2023 marked the beginning of a life-altering journey – one that would ultimately be defined not by fear, but by strength, resilience and the power of compassionate care. Determined to take control, Heather quickly decided on a course of action that would give her and her family the best chance at peace of mind.
She turned to Dr. Kayla Griffith at HCA HealthONE Rose, whose reputation and compassionate approach immediately put Heather at ease. “She walked in, confidently wearing pearls and cowboy boots,” Heather recalled. “I knew I was in the right place.” The team eased some of Heather’s fears and worries immediately. “It was the first time that anyone had taken the time to mention to me, ‘You are going to be okay,’ and I was so grateful to hear those simple words.”
Together, they decided on a double mastectomy with direct-to-implant reconstruction, a procedure that involves removing both breasts, then immediately placing breast implants during the same surgery. Heather felt confident in the decision thanks to the clear communication and support from her care team.
From diagnosis to surgery, only six weeks passed. On surgery day, Heather felt strong and supported. “[The team] knew what they were doing – no doubt about it – and the vibe they offered me on that day was one of hope for the future ahead of me.” Heather emphasized that it wasn’t just their medical expertise that made the difference – it was their empathy, communication and unwavering support.
Today, Heather is 18 months post-op and has completed 12 weeks of chemotherapy and five weeks of radiation. Reflecting on her journey, Heather says the day she was diagnosed was the scariest of her life. But meeting Dr. Griffith gave her the strength not just to fight – but to win. “What they are providing is empowerment in the face of a very scary cancer diagnosis.”
Stories of strength: Virginia nurses build lifelong bond through breast cancer journey


When Jenifer Hughes, a cardiac care nurse at HCA Healthcare’s Chippenham Hospital in Richmond, Virginia, was diagnosed with Stage 2 breast cancer, she braced for a difficult road ahead. At her first chemotherapy appointment at nearby HCA Healthcare affiliate Johnston-Willis Hospital, she met Alyssa Taylor, an oncology nurse and fellow Powhatan resident. But just two months later, their connection deepened in an unimaginable way – Alyssa was also diagnosed with Stage 2 breast cancer.
What began as a chance meeting became a powerful friendship. “It’s a bond nobody wants, but that bond lasts – and that’s huge,” Jenifer said.
Jenifer and Alyssa supported each other through treatment, sharing rides, meals and even creating “hydration games” to lighten the mood. They also joined a breast cancer support group at The Hawthorne Cancer Center, part of the Sarah Cannon Cancer Network at Johnston-Willis Hospital, and often met for food and laughter before sessions.
Their bond extended beyond support groups and hospital walls. When Jenifer was nominated for a day on the water through Sailing Beyond Cancer, she brought Alyssa and fellow survivors from Chippenham Hospital, turning the experience into a celebration of strength.
In July, Jenifer completed immunotherapy and was declared cancer-free; Alyssa followed in September, ringing the bell to mark the end of her treatment. For the duo, survivorship means more than just being cancer-free – it means carrying forward a friendship forged in resilience, compassion and hope.
Related article: Best friends and fellow nurses beat breast cancer side-by-side
link